Welcome to Diabetes Prevention Thursdays! Today, let’s talk about the biotechnical race to cure diabetes – part 2. Some advancements in research have potentially brought us closer to the goal of finding a cure or better method of treating type one (T1D) and type two diabetes (T2D). Both conditions can lead to serious complications. Let’s see what further developments are undergoing research now.
The Mexican Cavefish
What does a fish have to do with diabetes? This chubby, blind cave-dweller has evolved to be insulin resistant. Intrigue abounds when comparing the cave-dweller to its river-dwelling counterpart from the same species.
Insulin is released from the pancreatic B cells after eating, and this regulatory hormone latches onto receptors in your muscles, liver, and fat. Insulin absorbs the glucose from carbohydrates in the bloodstream into the cells. Your blood glucose levels normalize, and some glucose is burned for energy while some is stored as glycogen for later use. When your body starves, the pancreas releases glucagon, which converts glycogen back to glucose for energy.
Biologist Misty Riddle from the Stowers Institute for Medical Research examined the cave-dwelling fish closely to understand how it survived in its environment if it was insulin resistant. The cave-dwellers glucose levels were up and down after eating and fasting for 21-days, much more so than the river-dwelling fish.
The cave-dwelling fish converted their proline amino acids to leucine amino acids, a phenomenon seen in cases of severe insulin resistance. These fish have evolved to be diabetic, but they’re also living longer than the river-dwelling fish, confirming that they’ve adopted alternative mechanisms to thrive even in their diabetic state.

The Mexican cavefish phenomenon provides a means to investigate how T2D patients could adapt their natural homeostasis and avoid complications of their underlying diabetes.
The Microbiome
The microbiome is the collection of bacteria that protects your stomach, and it has a role in hormone regulation and the immune system. Imbalances in this gut flora can be a source of problems in managing diabetes. Trials are currently underway to enhance the flora and add a variety of bacteria that could help diabetics restore gut flora imbalances.
Virgin Beta Cells
Islet transplant therapy is when clusters of pancreatic cells from donors are transplanted into diabetic patients so that they can produce insulin again. During recent research, astonishing evidence was found of a new type of cell in the pancreatic islets clusters, which are the cells attacked and depleted in T1D. Among the clusters were immature beta cells, also called “virgin beta cells.” The question was whether these previously unnoticed cells could be matured to function as insulin-producing cells.
Mark Huising from the University of California and his colleagues are currently researching the virgin cells to determine whether they can be matured to respond to glucose levels in the bloodstream and release the necessary insulin. The immature beta cells lack the receptors to determine blood glucose levels. Further research will be needed to determine if these cells can subsequently develop these receptors and become fully functional.
Artificial Pancreas
A few different types of artificial pancreas exist today. Insulin pumps and the apps that work with them help parents monitor and care for children with T1D. The apps monitor glucose levels, and the pump automatically injects the right dose. The concept of the artificial pancreas is to replace the organ with newly placed virgin beta cells that are manipulated to prevent the immune system from attacking them. Researchers are still faced with two of the biggest problems: The scarcity of donors making it hard to conduct human trials and overcoming the immune system response to the virgin beta cells.
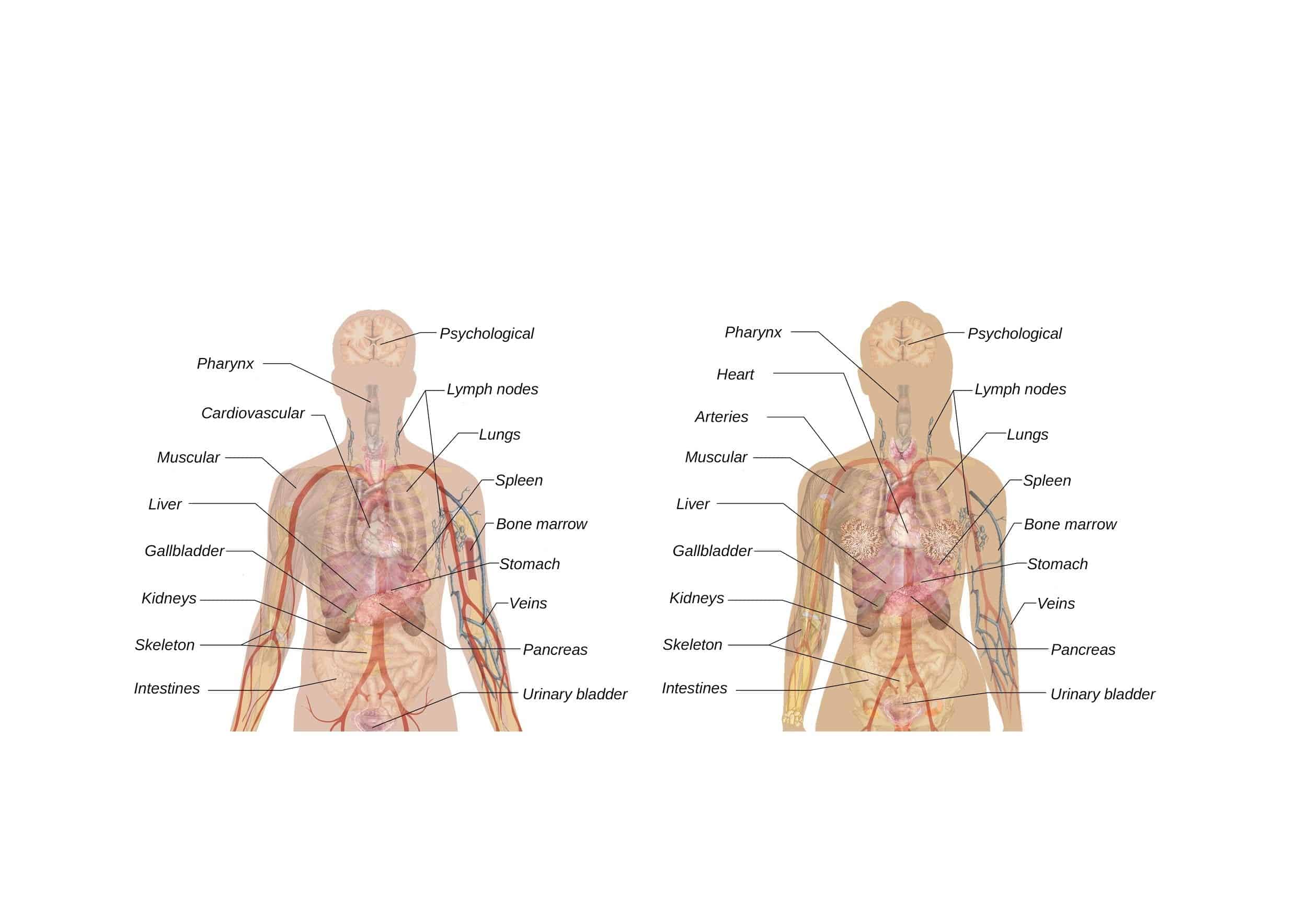
However, a new bioengineered pancreas was tested in a different body location, and the results from one woman’s improved T1D showed some success. The female T1D patient had the artificial organ transplanted into her omentum, and she had improvement of her T1D. The omentum is a large, flat tissue made of a fatty membrane in front of the intestines. The artificial organ in that region mimicked the pancreas more successfully than other transplant sites. Improvement in three areas will be beneficial in the advancement of the artificial pancreas:
- Faster-acting insulin.
- The use of Amylin, another hormone that improves the activity of insulin.
- Improving insulin dose algorithms.
Great strides have been made so far, but overcoming these problems will be a considerable advance in the treatment and methodology of curing T1D.
Food For Thought
Learning from nature always helps science advance in treating chronic conditions, and the success of various therapy trials continues to grow. There might not be a cure for diabetes today, but the future holds promise for millions of people globally.
If you would like to receive a free resource sheet to help you take control of diabetes, click the button below to receive your gift.
I wanted to talk about this topic because it is absolutely possible to prevent and even reverse Type 2 Diabetes (but you cannot reverse Type 1). Yes, it’s possible! and emerging studies looking at lifestyle medicine and prevention support this! But I always tell my patients that you must be dedicated and diligent in adopting a healthy lifestyle to get the best results. You can create certain behaviors and practices that will not only enrich your life, but that you can pass on to your family, friends, and community, to help break the cycle of this chronic disease so that you can leave a legacy of health to your loved ones.
I use functional medicine and lifestyle medicine as the first line of treatment, before medications, to treat lifestyle-related chronic diseases. Lifestyle-related chronic diseases include diabetes, hypertension, obesity, and some cancers, just to name a few. Lifestyle practices, such as eating a low glycemic, whole-food plant-based diet and regular physical activity, can help you improve your blood sugar levels, maybe reverse type 2 diabetes. In certain cases, these approaches may even outperform pharmaceutical therapy.
But I always tell my patients that conventional medications may be appropriate at this time to prevent catastrophic illness, but over time, you can work to make the necessary lifestyle changes to possibly reduce and/or eliminate medications. Please remember to always consult your physician for your particular needs and circumstances prior to making any decisions whatsoever.
Is Dietary Supplementation Right For You?
When it comes to managing your blood sugars (in general), pre-diabetes, and diabetes, there are many things that you can do to help control your blood sugar levels. One important aspect is diet. What you eat affects your blood sugar, so it’s important to be mindful of what goes into your body.
But it is very important to note that we are not eating the same foods we ate years ago because the soils have been depleted of critical nutrients through current industrial farming practices. And because the soil is not as good as it used to be, the food supply (grown from the depleted soil) is not as good as it used to be. For example, you are not getting the same levels of chromium and magnesium as you would have gotten 30 or even 50 years ago.
Second, much of the food has been processed and genetically altered, which can impact the inherent and unique nutritional composition that each food possess. For example, ancient einkorn wheat has less gluten, more protein, more Vitamin A, and more beta carotene, than modern genetically modified wheat.
Third, the toxic load in the environment today is much higher than 100 years ago. We can see this with global warming, toxic landfills, polluted oceans and waterways, etc. Toxicity levels interfere with nutrient assimilation and absorption not just into the foods, but into our bodies as well. We often see elevated blood sugar levels with poor nutrition and toxicity.
In addition to diet, there are dietary supplements that can have an impact on blood sugar levels. Dietary supplements for diabetes are becoming increasingly popular as people look for ways to improve their blood sugar control.
For some people, vitamin and mineral supplements offer important health benefits. Supplements are designed to fight deficiencies found in our diet and complement the food we eat regularly. Supplements are basically “helping hands” to our daily food.
If you suspect that you aren’t getting the nutrients you need, consider shifting your focus from supplements to eating better.
And if you are unable to eat better, the supplements in my Blood Sugar Support Bundle may provide the extra boost you need.
These are my favorite Diabetes Prevention Supplements to use! This Blood Sugar Support Bundle will ensure you have the intake of the important vitamins, minerals, and probiotics to decrease inflammation and boost your innate wellness day and night. Taken together, it’s a solid plan for increasing your body’s natural resiliency while encouraging healthy blood sugar levels.
For best results make sure you use these supplements with dietary changes including a whole food plant-based diet, regular exercise (at least 2-3x per week), regular sleep (8 hours per night), and intermittent fasting (at least 1-3x per week).
It’s important to note that supplements are NOT a replacement for your regular medication regimen prescribed by your doctor. However, they can be used in addition to help manage your blood sugar levels.
Supplements have the potential to interact with diabetes medications, so it’s important to speak with a healthcare provider before starting any new supplement regimen. Have you tried any dietary supplements for your diabetes? Share your experience in the comments below!
Tools For Diabetes Prevention and Monitoring
Blood Sugar Monitoring
As you know, I always stress the importance of taking control of your health. Monitoring your blood sugar levels is one of the best ways to do this. To do this, a single drop of blood is collected with disposable lancets and placed on a disposable test strip, which you insert into a home blood-sugar monitoring device, called a glucometer.
The common times for checking your blood sugar are when you first wake up (fasting), before a meal, 2 hours after a meal, and at bedtime; however, you should check your blood sugar as many times a day as your health care team suggests.
Monitoring your blood sugar level provides you and your doctors with important knowledge about how food, activity, medication, stress, and other elements might affect your blood sugar levels. This data will assist you and your doctor in developing a therapy plan that is suited to your demands.
There are several types of blood glucose meters, lancets, and test strips to choose from. I often recommend this glucometer, lancets, and test strips.
Weight Monitoring
Since weight management is very important in combatting chronic diseases such as diabetes, I recommend that you be mindful of your weight and its fluctuations, and that you monitor your weight AT LEAST on a weekly basis. I recommend a scale that includes a body composition monitor (*this scale cannot be used with a pacemaker or other implanted devices).
Physical Activity
Physical activity (or exercise) can improve your health and reduce the risk of developing several chronic diseases like high blood pressure, type 2 diabetes, and cancer, just to name a few. Physical activity actually improves insulin sensitivity. Physical activity can improve your mood, boost your immune system, and even help you maintain a healthy weight.
I often recommend yoga and resistance training for physical activity, but as you are aware, there are plenty of forms of “movement” that you can do! But for the basics, especially if you’re just getting started, yoga and resistance training are where I would start.
Yoga
Yoga can be a great way to improve your strength and flexibility, manage your stress, improve your heart health, and lose weight! I recommend using this yoga mat to get started with your yoga practice today!
Resistance Training
Resistance training is the mainstay for overall health. It not only has beneficial effects on reducing body fat, it also increases muscle size and strength. Here are some basic resistance bands that I recommend to everyone. They are great for physical therapy, yoga, strength training, and excellent for traveling.
Food!
Remember, living a healthy lifestyle including eating a whole foods plant-based diet and regular physical activity are the best ways to prevent diabetes.
The Diabetes Meal Plan is geared towards those people with diabetes or prediabetes. The foods are moderately low in carbs, low glycemic, fiber rich, and contain a balance of nutrients to help prevent blood sugar spikes and dips. Foods are also included that may help to lower blood sugar.
Please talk with your doctor about any complementary health approaches, including supplements, you use.
Dr. Nicolle Martin
Some of the links in this article are "affiliate links", a link with a special tracking code. This means if you click on an affiliate link and purchase the item, we will receive an affiliate commission.
The price of the item is the same whether it is an affiliate link or not. Regardless, we only recommend products or services we believe will add value to our readers.
By using the affiliate links, you are helping support our Website, and we genuinely appreciate your support.
Last updated on January 28th, 2022 at 06:57 am
Minimize Medications. Maximize Health.
Are you super busy but need to take control of your health? Are you tired of being tired? Subscribe to my “Minimize Medications, Maximize Health Blog” and I’ll give you 7 Tips to Get Healthy in No Time absolutely FREE.