It was a cold and rainy day in the city, and Dr. Nicolle had just finished another long shift at the hospital. She was exhausted, physically and emotionally, after seeing patient after patient with preventable illnesses and conditions.
As she trudged through the rain towards her car, her thoughts turned to the patients she had seen that day – the elderly man with diabetes who couldn’t afford his insulin, the young woman with asthma who had to choose between paying for her medication or putting food on the table.
“I can’t keep doing this,” she muttered to herself, feeling overwhelmed by the magnitude of the problem. “There has to be a way to make things better.”
As she unlocked her car door, her phone buzzed in her pocket. It was a message from one of her colleagues, Dr. Rodriguez.
“Hey, Nicolle, have you seen the latest statistics on health disparities in our city?” the message read.
Dr. Nicolle felt a spark of hope in her chest. “No, I haven’t,” she replied. “What do they say?”
Dr. Rodriguez sent her a link to a report on health equity in their city, and as Dr. Nicolle read through the data, she felt her heart sink. The numbers were even worse than she had imagined – people of color and low-income individuals were disproportionately affected by preventable diseases and illnesses, with limited access to quality healthcare.
“This can’t be happening,” she said, her voice shaking with anger. “We have to do something about this.”
And with that, Dr. Nicolle and Dr. Rodriguez set out to create a plan for improving health equity and inclusion in their city. They spent months researching and strategizing, working tirelessly to bring their vision to life.
And now, as they prepare to launch their new initiative, Dr. Nicolle feels a sense of hope and purpose that she hasn’t felt in a long time.
“We can make a real difference,” she says, her eyes shining with determination. “We can create a healthcare system that serves everyone, regardless of their background or circumstances. And I truly believe that we will.”
Continue reading below…

Health Equity and Inclusion is a crucial aspect of modern healthcare, aiming to eliminate disparities and improve health outcomes for all. Busy professionals must recognize the elements that affect their wellbeing and gain knowledge on how to manage their health. This blog post will explore various dimensions of health equity and inclusion and provide valuable insights into addressing these challenges.
We’ll delve into the social determinants of health, examining the role socioeconomic status plays in healthcare access and how education impacts health literacy. Additionally, we’ll discuss environmental factors affecting immune resilience, highlighting common sources of exposure to toxins and strategies for reducing them at home or workplace.
Furthermore, this post will address healthcare barriers faced by BIPOC populations with an emphasis on disparities in diagnosis and treatment options available to minority groups. We’ll also look at pandemic-related challenges exacerbating chronic stress and their effects on physical and mental health within marginalized communities.
Lastly, we’ll cover functional medicine approaches promoting Health Equity Inclusion through tailored food plans according to cultural preferences as well as community-based programs encouraging healthy habits. The role of subject matter experts in interdisciplinary collaboration efforts aimed at addressing inequities will also be discussed along with examples of successful initiatives led by such experts.
Minimize Medications. Maximize Health.
Are you super busy but need to take control of your health? Are you tired of being tired? Subscribe to my “Minimize Medications, Maximize Health Blog” and I’ll give you 7 Tips to Get Healthy in No Time absolutely FREE.
You have Successfully Subscribed!
Social Determinants of Health
When it comes to achieving health equity, addressing the social determinants of health is critical. These factors are the conditions in which people are born, live, learn, work, play, worship, and age. They greatly impact a wide range of health outcomes and risks. By understanding these social determinants and their influence on healthcare access and quality for different populations, we can create more inclusive solutions that advance health equity.
Understanding the Role of Socioeconomic Status in Healthcare Access
Socioeconomic status (SES) plays a significant role in determining an individual’s access to quality healthcare services. Lower SES often translates into limited financial resources or inadequate insurance coverage, which may result in delayed care or avoidance altogether due to cost concerns. This leads to poorer overall health outcomes. To improve health equity among various income levels:
- Policymakers should consider implementing policies that address affordability barriers such as expanding Medicaid eligibility.
- Health systems could offer sliding-scale payment options based on patients’ ability to pay.
- Educational initiatives aimed at improving financial literacy might help individuals make informed decisions about purchasing appropriate insurance coverage.
The Influence of Education on Health Literacy
A person’s level of education has been shown to be closely linked with their overall health literacy, i.e., their ability to understand basic information about maintaining good health or managing existing health conditions. Lower levels of education are often associated with lower health literacy, which can lead to difficulty navigating the healthcare system and making informed decisions about one’s care. To address this issue:
- Healthcare providers should be trained in effective communication techniques that cater to varying degrees of health literacy.
- Schools could incorporate comprehensive health education programs into their curricula from an early age.
- Community-based organizations might offer workshops or classes on topics such as disease prevention, nutrition, and self-care strategies for individuals who may have missed out on formal education opportunities.
Incorporating these approaches within our communities will help bridge the gap between different socioeconomic groups and ensure everyone has equal access to quality healthcare services – a crucial step towards achieving true health equity inclusion for all. Addressing health equity is especially important during the COVID-19 pandemic, as it has highlighted and exacerbated existing health disparities and inequities.
By eliminating disparities and advancing health equity, we can improve health outcomes for vulnerable populations and influence disease prevention and control. It is up to all of us, including policy makers, healthcare providers, and community members, to work together to advance health equity and address food insecurity, social determinants, and other factors that impact health outcomes.
Socioeconomic status can significantly impact individuals’ health, making it necessary to comprehend the implications of social determinants on access and outcomes in healthcare. By understanding environmental factors affecting immune resilience, we can work towards reducing exposure to toxins and improving our health through lifestyle changes.
Key Thought:
To achieve health equity inclusion, it is crucial to address social determinants of health that impact healthcare access and quality for different populations. Socioeconomic position has a major effect on an individual’s ability to access healthcare of high quality, while educational level can shape general health knowledge. Policymakers, healthcare providers, schools and community-based organizations should work together to bridge the gap between socioeconomic groups by implementing policies that address affordability barriers and offering effective communication techniques catered towards varying degrees of health literacy.
Environmental Factors Affecting Immune Resilience
Did you know that exposure to environmental toxins can significantly impact your immune resilience? It’s true. Toxins such as heavy metals, pesticides, ambient pollutants, and endocrine-disrupting chemicals have been shown to negatively affect our body’s ability to fight off infections and maintain overall health. Unfortunately, these factors are often more prevalent in communities disproportionately affected by them (e.g., BIPOC populations), leading to increased disparities in chronic disease prevalence.
Identifying Common Sources of Exposure to Environmental Toxins
- Air pollution: Emissions from factories, vehicles, and power plants contribute significantly to poor air quality. Living near highways or industrial areas increases the risk of exposure.
- Pesticides: Agricultural workers may be exposed directly through handling pesticides; however, residues on fruits and vegetables can also pose a risk for consumers if not properly washed. Agricultural practices often involve using chemical pesticides on crops which can contaminate soil and water supplies.
- Heavy metals: Contaminated water sources or old plumbing systems can lead to ingestion of heavy metals like lead. Additionally, some fish species accumulate high levels of mercury due to human activities.
- Hazardous waste sites: Communities located near landfills or other waste disposal facilities may face higher risks due to contaminated soil or groundwater.
- Endocrine disruptors: Chemicals like bisphenol-A (BPA), commonly found in plastic products or canned food linings, may interfere with hormone regulation leading to adverse health effects.
TIP: The United States Environmental Protection Agency (EPA) provides an interactive tool called “EJSCREEN: Environmental Justice Screening and Mapping Tool” which allows users to explore potential environmental risks within their communities based on location data.
Strategies for Reducing Exposure at Home or Workplace
While we can’t eliminate all environmental toxins from our lives, there are steps you can take to reduce your exposure and protect your immune resilience:
- Improve indoor air quality: Use air purifiers with HEPA filters, regularly change HVAC filters, keep windows open when possible for ventilation, and avoid smoking indoors.
- Eat organic produce: Choosing organic fruits and vegetables whenever possible can help minimize pesticide residues. Don’t forget to wash them thoroughly. You can also check out the Environmental Working Group’s (EWG) Dirty Dozen list for guidance on which produce items are most likely to be contaminated with pesticides.
- Test water sources: Regularly test your home’s tap water for contaminants like lead or other heavy metals. Consider using a certified water filter if necessary.
- Promote workplace safety: Advocate for proper handling of hazardous materials at work, including training on safe disposal methods and use of personal protective equipment (PPE).
- Avoid lead exposure: Test your home for lead-based paint or water contamination if it was built before 1978. If necessary, take steps like using certified water filters or hiring professionals for safe removal of lead-containing materials.
- Limited use of plastics: Reduce reliance on plastic products by opting for glass or stainless steel containers and avoiding canned foods with BPA linings when possible.
Taking these measures not only helps improve health equity by addressing the disproportionate impact of environmental factors on BIPOC populations but also benefits everyone in their quest for better health outcomes. Remember: a cleaner environment means healthier communities.
It is critical to recognize the ecological elements that can influence invulnerable strength, as this comprehension can help us settle on educated choices about our wellbeing. Healthcare barriers faced by BIPOC populations are a serious issue and require further exploration in order to reduce disparities in diagnosis and treatment options available.
Key Thought:
Exposure to environmental toxins can negatively impact our immune resilience, with BIPOC communities being disproportionately affected. Air pollution, pesticides, heavy metals and endocrine-disrupting compounds are all sources of exposure that can adversely affect immune function; particularly in BIPOC communities. To reduce exposure at home or work environments we can improve indoor air quality, eat organic produce and limit the use of plastics among other strategies.
Healthcare Barriers Faced by BIPOC Populations
Black, Indigenous, and People of Color (BIPOC) face significant barriers when accessing quality healthcare services. This results in higher rates of chronic illnesses among these populations compared to their white counterparts. Recognizing these challenges is essential for creating inclusive solutions that address systemic inequalities.
Disparities in Diagnosis and Treatment Options Available to Minority Groups
The unfortunate reality is that health disparities exist across racial and ethnic lines. For instance, BIPOC individuals are more likely to experience delayed diagnoses or receive inadequate treatment options for various health conditions such as cancer, diabetes, heart disease, and mental health disorders. Bias, cultural competency gaps, language obstacles and restricted access to care based on geography or insurance can all contribute to the health disparities experienced by BIPOC individuals.
- Solution: Policy makers should prioritize efforts aimed at eliminating disparities through targeted interventions like increasing funding for community-based programs that provide culturally sensitive education on disease prevention and control.
Impact on Mental Wellbeing Due to Limited Access or Inadequate Care
Mental health is an integral aspect of overall well-being; however, mental health disparities persist among minority groups, particularly those who identify as BIPOC. Lack of access to culturally competent mental healthcare professionals may lead many people from marginalized communities feeling unheard or misunderstood during therapy sessions – ultimately resulting in suboptimal outcomes, increased feelings of isolation, depression, anxiety, and other related issues which only serve to exacerbate existing problems and further perpetuate the cycle of disparity experienced by members of this population segment throughout America today.
The COVID-19 pandemic has further exacerbated this issue with increased isolation leading many individuals experiencing heightened levels of anxiety or depression without adequate support systems available. Furthermore, language differences can impede access to mental health services and comprehension of treatment options for non-English speakers.
- Solution: Health systems should invest in language assistance programs, telehealth services, and culturally competent care providers to improve communication between healthcare professionals and BIPOC patients. To ensure equitable access to healthcare, it is essential to invest in targeted interventions that address the language and cultural barriers faced by BIPOC populations.
Addressing Healthcare Barriers: Steps Towards Health Equity
To advance health equity and improve the healthcare experience for BIPOC populations, it is crucial to address these barriers head-on. Here are some strategies that can help:
- Cultural Competence Training: Ensuring that healthcare providers receive adequate training in cultural competence can lead to a better understanding of patients’ unique needs and experiences, ultimately improving patient-provider relationships and treatment outcomes.
- Community Outreach Programs: Implementing community-based programs focused on disease prevention, early detection, and access to care can help bridge gaps in service delivery for marginalized communities.
- Patient Advocacy: Encouraging individuals from diverse backgrounds to become advocates within their own communities can foster a sense of empowerment and promote positive change in local healthcare systems.
- Inclusive Policy Making: Engaging policy makers at all levels of government is essential for creating policies that prioritize addressing health disparities and promoting equitable access to quality medical services regardless of race, ethnicity, income level, or other identifying characteristics which may otherwise limit one’s ability to receive the proper attention needed during times of illness, recovery, and wellness maintenance alike (Healthy People 2030).
Influencing health outcomes positively by addressing the barriers faced by BIPOC populations requires a multifaceted approach. Through recognizing and engaging with the difficulties experienced by BIPOC groups, we can further health equity and create a comprehensive healthcare system in which all individuals have an equal chance to succeed.
The healthcare disparities faced by BIPOC populations are a major issue that must be addressed. To further explore the effects of these barriers, it is important to consider how pandemic-related challenges have exacerbated chronic stress in marginalized communities.
Key Thought:
BIPOC populations face significant healthcare barriers, resulting in higher rates of chronic illnesses compared to their white counterparts. Discrepancies in the identification and available treatments, as well as restricted access or substandard care for mental health concerns, are contributing to these problems. Strategies such as cultural competence training for healthcare providers, community outreach programs focused on disease prevention and early detection, patient advocacy, and inclusive policy-making can help address these barriers towards advancing health equity.
Pandemic-related Challenges Exacerbating Chronic Stress
The COVID-19 pandemic has brought about additional stressors such as job loss concerns, difficulties obtaining necessary healthcare services, food insecurity, and housing instability. These challenges impact already elevated levels of anxiety experienced within marginalized communities, like those who identify themselves as being part of Black, Indigenous, and People of Color (BIPOC) groupings across America. Today, more than ever before, it’s important to recognize how our current environment exacerbates existing disparities so we may better support individuals facing unique struggles during this time period, particularly related to areas where there exists a high prevalence of chronic stress conditions.
Effects of Increased Stress on Physical and Mental Health
Cortisol, a hormone released in response to chronic stress, can have numerous negative health consequences such as obesity, heart disease, diabetes, depression and anxiety disorders. For BIPOC populations who face systemic barriers in accessing quality healthcare services or experience discrimination within the system itself, these negative outcomes may be further exacerbated due to limited resources available for managing their overall well-being.
Strategies for Managing Pandemic-related Stressors in Marginalized Communities
To mitigate the harmful effects that pandemic-related challenges pose on the mental wellbeing of vulnerable populations like BIPOC communities, several strategies can be employed:
- Educate about coping mechanisms: Providing information on effective ways to manage daily stresses through self-care practices such as mindfulness meditation or regular exercise can empower individuals to take control over their emotional well-being even amidst difficult circumstances.
- Increase access to telehealth services: Expanding availability for remote consultations with healthcare professionals allows patients from marginalized communities to receive necessary care without risking exposure to COVID-19 or facing transportation barriers. Telehealth services have proven effective in improving health outcomes and reducing disparities during the pandemic.
- Support community-based initiatives: Partnering with local organizations that address food insecurity, housing instability, and other social determinants of health can help alleviate some of the stressors faced by marginalized populations during this time.
- Promote mental health resources: Ensuring access to culturally sensitive mental health resources such as therapy sessions or support groups tailored for BIPOC individuals can provide a safe space for them to discuss their unique experiences and challenges related to the pandemic.
Incorporating these strategies into healthcare systems will not only aid in managing pandemic-related stressors but also contribute towards advancing health equity within our society by addressing underlying systemic issues affecting vulnerable populations like BIPOC communities.
The pandemic has increased stress levels among many individuals, especially those in marginalized communities. As a result, Functional Medicine approaches to health equity can help reduce chronic stress by tailoring food plans according to cultural preferences and encouraging healthy habits through community-based programs.
Key Thought:
The COVID-19 pandemic has exacerbated chronic stress conditions in marginalized communities, particularly those who identify as BIPOC. Increased stress can have detrimental effects on physical and mental health, but strategies such as educating about coping mechanisms, increasing access to telehealth services, supporting community-based initiatives, and promoting culturally sensitive mental health resources can help manage pandemic-related stressors and advance health equity within our society.
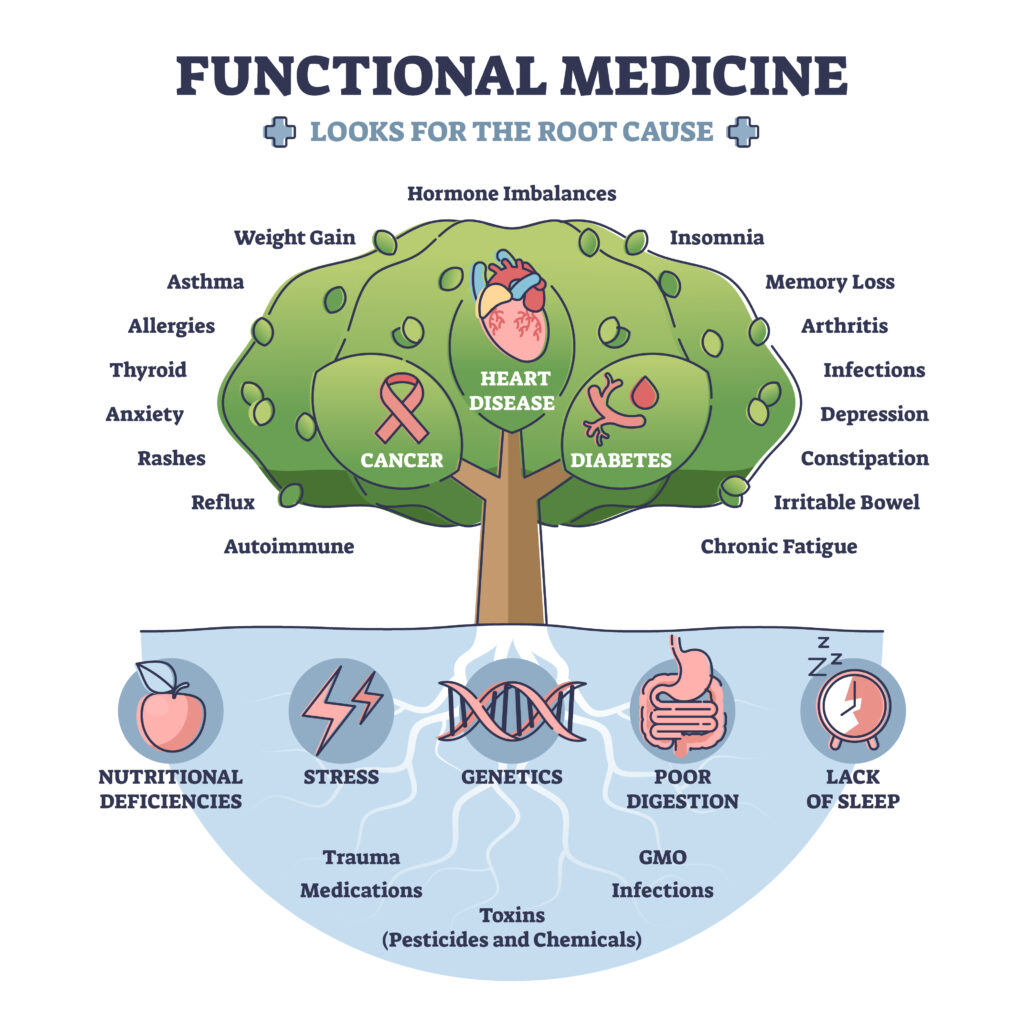
Functional Medicine Approaches to Health Equity
A functional medicine approach can help address health disparities by focusing on individualized care that considers lifestyle factors, cultural background, and specific needs. Collaboration and trust between patients and practitioners are essential components for creating a more inclusive healthcare system.
Tailoring Food Plans According to Cultural Preferences
Eating habits play a significant role in overall health, but traditional dietary recommendations often fail to consider the diverse cultural backgrounds of individuals. Functional medicine practitioners recognize this gap and work with patients to develop personalized food plans that respect their heritage while promoting optimal nutrition. By incorporating familiar ingredients from various cuisines, these tailored food plans not only support better health outcomes but also encourage adherence by making healthy eating enjoyable and sustainable.
Encouraging Healthy Habits Through Community-Based Programs
To advance health equity at a larger scale, functional medicine practitioners collaborate with community organizations to design programs that promote healthy lifestyles among vulnerable populations. These initiatives may include:
- Disease prevention workshops: Educating communities about risk factors associated with chronic diseases like diabetes or heart disease empowers them to make informed decisions regarding their well-being.
- Fitness classes: Offering accessible physical activity options within local neighborhoods encourages regular exercise as part of daily routines.
- Nutrition education sessions: Providing practical information on how families can prepare affordable yet nutritious meals helps combat food insecurity issues faced by many marginalized groups.
- Mental wellness resources: Addressing mental health concerns through culturally sensitive counseling services supports holistic healing beyond just physical ailments.
Incorporating functional medicine approaches into community-based programs can improve health equity by addressing the unique needs of diverse populations. By fostering collaboration between patients, practitioners, and local organizations, these initiatives create lasting change in communities disproportionately affected by health disparities.
Functional Medicine approaches to health equity are an important part of improving the overall health and wellbeing of underserved communities. By involving subject matter experts in promoting health equity, we can ensure that these initiatives have a greater impact on closing existing gaps in access to healthcare.
Key Thought:
Functional medicine practitioners can help address health disparities by tailoring individualized care that considers lifestyle factors, cultural background, and specific needs. They work with patients to develop personalized food plans that respect their heritage while promoting optimal nutrition and collaborate with community organizations to design programs that promote healthy lifestyles among vulnerable populations. By fostering collaboration between patients, practitioners, and local organizations through culturally sensitive counseling services, these initiatives create lasting change in communities disproportionately affected by health disparities.
The Role of Subject Matter Experts in Promoting Health Equity
Subject matter experts play an important role in promoting health equity by doing the following:
- sharing their knowledge about social determinants, environmental factors, barriers faced by BIPOC populations,
- discussing strategies used within functional medicine aimed at reducing these gaps among different groups living across America,
- and by ensuring that everyone has equal access to opportunities when seeking out quality medical services, regardless of race, ethnicity, income level, or other identifying characteristics that may otherwise limit one’s ability to receive proper attention needed during times of illness, recovery, wellness, and maintenance alike.
Importance of Interdisciplinary Collaboration for Addressing Health Inequities
In order to effectively address health inequities and advance health equity, it is crucial for subject matter experts from various disciplines such as healthcare providers, policy makers, researchers, and community leaders to collaborate on initiatives focused on improving health outcomes. For example, the Center for Global Policy Solutions’ Health Equity Initiative brings together professionals from diverse backgrounds with the goal of eliminating disparities through research-driven policy recommendations.
Examples of Successful Initiatives Led by Subject Matter Experts
- Racial Healing Circles: Driven by renowned expert Dr. Gail Christopher, Racial Healing Circles provide safe spaces where individuals can engage in honest conversations about race-related issues while working towards healing historical wounds caused by systemic racism.
- Fighting Food Insecurity: Registered dietitian and food justice advocate Clancy Harrison works tirelessly to address food insecurity by educating healthcare professionals on the importance of recognizing and addressing this issue in their practice, as well as through her non-profit organization, the Food Dignity Project.
- Covid-19 Pandemic Response: Experts like Dr. Shanta Zimmer, MD have been instrumental in guiding policy makers during the Covid-19 pandemic to ensure that vulnerable populations receive adequate care and support throughout these challenging times. Her work has focused on disease prevention and control measures tailored specifically for marginalized communities disproportionately affected by the virus.
By leveraging their expertise, subject matter experts play a vital role in driving change towards a more equitable healthcare system. Through interdisciplinary collaboration and targeted initiatives, they are helping improve health outcomes for all individuals regardless of race or socioeconomic status.
Key Thought:
Subject matter experts play a crucial role in promoting health equity by sharing their knowledge and collaborating with other professionals to address health inequities. Successful initiatives led by subject matter experts include Racial Healing Circles, fighting food insecurity, and guiding policy makers during the Covid-19 pandemic to ensure vulnerable populations receive adequate care and support.
I would love to give you a free resource sheet to support your overall wellness. Click the button below to receive your gift.
I really wanted to talk about this topic today because your natural health and wellness is important. You can adopt healthy lifestyle practices that improve your health, your environment, and enrich your life, which can in turn improve the lives of those close to you. You have the power to break the cycle of poor health, including chronic disease, so that you can leave a legacy of health to your loved ones.
I use functional medicine and lifestyle medicine as the first line of treatment, before medications, to treat lifestyle-related chronic diseases. Lifestyle-related chronic diseases include diabetes, hypertension, obesity, and some cancers, just to name a few. Lifestyle practices, such as eating a whole-food plant-based diet and regular physical activity, can help you lose weight, reverse some chronic diseases (if you suffer from them), and can even help you with detoxification. In certain cases, these approaches may even outperform pharmaceutical therapy.
But I always tell my patients that conventional medications may be appropriate at this time to prevent catastrophic illness, but over time, you can work to make the necessary lifestyle changes to possibly reduce and/or eliminate medications. Please remember to always consult your physician for your particular needs and circumstances prior to making any decisions whatsoever.
Is Dietary Supplementation Right For You?
For some people, vitamin and mineral supplements offer important health benefits. Supplements are designed to fight deficiencies found in our diet and complement the food we eat regularly. Supplements are basically “helping hands” to our daily food.
If you suspect that you aren’t getting the nutrients you need, consider shifting your focus from supplements to eating better.
But it is very important to note that we are not eating the same foods we ate years ago because the soils have been depleted of critical nutrients through current industrial farming practices. And because the soil is not as good as it used to be, the food supply (grown from the depleted soil) is not as good as it used to be. For example, you are not getting the same levels of magnesium as you would have gotten 30 or even 50 years ago.
Second, much of the food has been genetically altered, which can impact the inherent and unique nutritional composition that each food possess. For example, ancient einkorn wheat has less gluten, more protein, more Vitamin A, and more beta carotene, than modern genetically modified wheat.
Third, the toxic load in the environment today is much higher than 100 years ago. We can see this with global warming, toxic landfills, polluted oceans and waterways, etc. Toxicity levels interfere with nutrient assimilation and absorption not just into the foods, but into our bodies as well.
So… if you are unable to eat better, the supplements in my MaxHealth Essentials Bundle may provide the extra boost you need.
These are my favorite Wellness and Immune-Boosting Supplements to use! This MaxHealth Essentials Bundle will ensure you have the intake of the important vitamins, minerals, and antioxidants to decrease inflammation and boost your innate wellness day and night. Taken together, it’s a solid plan for increasing your body’s natural resiliency.
For best results make sure you use the supplements with dietary changes including a whole food plant-based diet, regular exercise (at least 2-3x per week), regular sleep (8 hours per night), and intermittent fasting (at least 1-3x per week).
Weight Monitoring
Since weight management is very important in combatting chronic diseases, I recommend that you be mindful of your weight and its fluctuations, and that you monitor your weight AT LEAST on a weekly basis. I recommend a scale that includes a body composition monitor (*this scale cannot be used with a pacemaker or other implanted devices).
Physical Activity
Physical activity (or exercise) can improve your health and reduce the risk of developing several chronic diseases like high blood pressure, type 2 diabetes, and cancer, just to name a few. Physical activity can improve your mood, boost your immune system, help you maintain a healthy weight, and is a great way to detox your body!
I often recommend yoga and resistance training for physical activity, but as you are aware, there are plenty of forms of “movement” that you can do! But for the basics, especially if you’re just getting started, yoga and resistance training are where I would start.
Yoga
Yoga can be a great way to improve your strength and flexibility, manage your stress, improve your heart health, and lose weight! I recommend using a grounded yoga mat to connect yourself with the earth and reduce inflammation.
Resistance Training
Resistance training is the mainstay for overall health. It not only has beneficial effects on reducing body fat, it also increases muscle size and strength. Check out some basic dumbbells/free weights that I recommend to everyone.
Another alternative for dumbbells/free weights are resistance bands. They are great for physical therapy, yoga, strength training, and excellent for traveling.
Remember, living a healthy lifestyle including eating a whole foods plant-based diet, regular physical activity, and reducing stress are the best ways to maintain a healthy weight. Let me know what you think in the comment section below.
Health Equity Inclusion FAQs
Health equity refers to the fair distribution of resources, opportunities, and access to healthcare services for all individuals regardless of their social or economic status. Inclusion emphasizes the importance of involving diverse communities in decision-making processes related to healthcare policies and programs. Together, health equity and inclusion aim to reduce disparities in health outcomes among different population groups.
The 3 P’s of health equity include Place, People, and Power. ‘Place’ focuses on creating healthy environments by addressing factors such as housing conditions and air quality. ‘People’ highlights the need for equitable access to healthcare services across various demographic groups. ‘Power’ emphasizes empowering marginalized communities through advocacy efforts that promote equal representation in policy decisions affecting public health.
Inclusion supports health equity by ensuring that diverse perspectives are considered when developing policies or implementing interventions aimed at improving overall population well-being. By engaging underrepresented communities in decision-making processes, inclusive approaches can help identify barriers faced by these populations while also tailoring solutions according to their unique needs – ultimately leading towards more equitable outcomes.
A scholarly article on Health Equity is an academic publication authored by experts who have conducted research or reviewed existing literature related to promoting fairness within healthcare systems. One example is “Achieving Health Equity: From Root Causes To Fair Outcomes“, which discusses strategies for addressing underlying determinants contributing towards disparities in global public-health outcomes.
Final Thoughts
Understanding the social determinants of health, identifying environmental factors affecting immune resilience, and addressing healthcare barriers faced by BIPOC populations are crucial steps towards achieving Health Equity and Inclusion. The pandemic-related challenges exacerbating chronic stress can also be managed through functional medicine approaches and interdisciplinary collaboration led by subject matter experts.
In order to advance Health Equity Inclusion, we must take action in our communities by supporting initiatives that address health disparities and promote disease prevention. Dr. Nicolle Martin is a leading expert in functional medicine who specializes in helping individuals improve their health outcomes through personalized care plans that prioritize holistic wellness. Contact her today to learn more about how you can join the movement towards advancing Health Equity Inclusion!
Contact Dr. Nicolle Martin to start your journey towards better health!
Dr. Nicolle Martin
Some of the links in this article are "affiliate links", a link with a special tracking code. This means if you click on an affiliate link and purchase the item, we will receive an affiliate commission.
The price of the item is the same whether it is an affiliate link or not. Regardless, we only recommend products or services we believe will add value to our readers.
By using the affiliate links, you are helping support our Website, and we genuinely appreciate your support.
Last updated on October 18th, 2023 at 05:46 pm
Minimize Medications. Maximize Health.
Are you super busy but need to take control of your health? Are you tired of being tired? Subscribe to my “Minimize Medications, Maximize Health Blog” and I’ll give you 7 Tips to Get Healthy in No Time absolutely FREE.